We are getting a lot of questions here at Chandler Hall about the new COVID vaccines and how they will impact our residents and our community. We want to answer your questions here, to help everyone better understand what we know, what we expect, and what might be next.
When will the COVID-19 vaccine be available to senior living residents in Pennsylvania?
The short answer: we’re still waiting for an exact date. Our staff will monitor the vaccine rollout closely, so we can immediately give you an accurate answer to this critical question as soon as the information is available.
As it stands today, Long term Care Facility Residents are third in line according to an interim report published by the Pennsylvania Department of Health on December 11, 2020.
Critical Populations
- Healthcare personnel
- Other essential workers
- Long-term care facility residents
- People with underlying medical conditions that are risk factors for severe COVID-19
- illness
- People 65 years of age and older
- People from racial and ethnic minority groups
- People from tribal communities
- People who are incarcerated/detained in correctional facilities
- People experiencing homelessness/living in shelters
- People attending colleges/universities
- People living and working in other congregate settings
- People living in rural communities
- People with disabilities
- People who are under or uninsured
It is important to note that recommendations on the various population groups to receive initial doses of vaccine could change after the vaccine is available, depending on each vaccine’s characteristics, vaccine supply, disease epidemiology, and local community factors.
Prioritization of Vaccines here in Bucks County
Every State and County has to coordinate the distribution of vaccines. Priorities have been set as outlined above, but there is still much work to do to decide how to best distribute this precious vaccine to the greater community.
The Decisions We Face at Chandler Hall
There are other challenges we still have to face- Who gets first priority? Who is at highest risk for an adverse reaction? If a patient has cognitive issues in our memory care unit, for example, will the family members agree to have the resident vaccinated? Should we require vaccination of every resident and staff member? What happens if someone does not agree? Since some people experience some discomfort or some small effects the day after the vaccine, will this do more harm than good for some of our more medically fragile patients? How do we make sure we get all the vaccine we need- for the first and second doses? Which brand will we get? How long will it take to vaccinate everyone?
Hospitals, Health care centers, and senior communities all across the nation are struggling with these issues and trying to make the best decisions possible, even before the vaccine becomes readily available to them. We are in the process of trying to work through these issues ourselves, and consulting with other communities to come up with the best system possible. We will keep you up to date with any information we have, and help set expectations as soon as we have more concrete information.
I keep seeing information on all these different vaccines out there – some are approved, and some are not. What do I need to know?
Why do we need a Vaccine?
- The point of a vaccine is to help introduce your natural immune system to a virus or other pathogen in such a way that your system has antibodies in place to fight off any infection if you are ever exposed to the disease.
When you encounter a virus, bacteria, or other pathogen for the first time, your immune system has to create antibodies to fight the disease. When your immune system kicks into gear, you can often feel sick or not quite right – you might get a fever, feel tired, get a cough or a runny nose- all because your immune system is “turning on” all its protective mechanisms to fight off the invaders. The discomfort that you experience such as mucus and phlegm is produced by your body to essentially help catch and filter out dirt, dust and other foreign invaders. Fever is actually a signal to your body to turn on certain aspects of your immune system.
In extreme cases, your immune system can severely “over-react” to an invader, causing severe inflammation throughout your body and actually do damage- this is called “Cytokine storm” and it may be responsible for some of the deaths due to COVID-19.
A vaccine introduces your body to a pathogen in a safe way. It stimulates an immune response without triggering an over-reaction or illness. There are a variety of vaccine types including:
- Live Attenuated vaccine: this type of vaccine uses a weakened version of the virus or pathogen that usually gets you sick. Vaccines for chickenpox, measles, and rotavirus are examples of “live attenuated” vaccines. They often have to be kept cold, and one or two doses can give you lifetime immunity
- Inactivated Vaccines: These vaccines are based on a “killed” version of the pathogen in question, and they tend not to provide as strong of an immune response as attenuated vaccines. They inject a piece or specific part of a pathogen to generate an immune response. They often require boosters, but they are safer for people with compromised immune systems than live attenuated vaccines. These vaccines include HPV, Hepatitis B, Shingles, Whooping Cough, Pneumococcal disease and others.
- Toxiod Vaccines: These vaccines use a toxin made by the germ or pathogen, so you get an immune response to the “bad” stuff the pathogen causes, rather than to the germ itself. This is how the diphtheria and tetanus vaccines work, and they also require boosters to maintain immune responses.
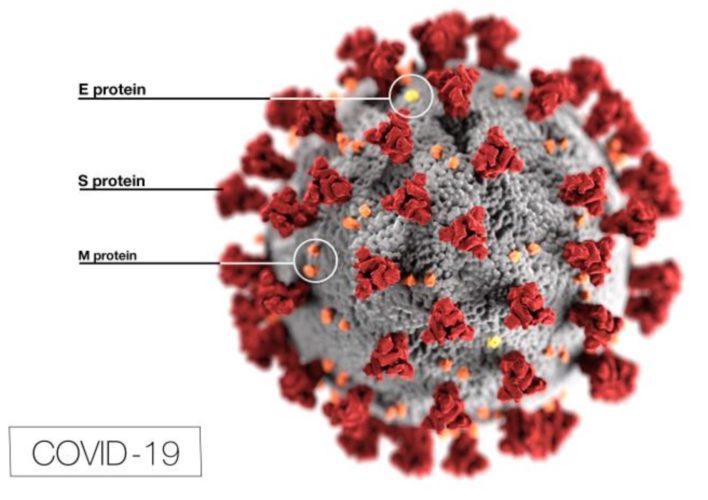
- DNA/mRNA vaccines: What is exciting about several of the new COVID-19 vaccines, is that they are using the virus’s own genetic code against it. The Pfizer and Moderna vaccine are messenger RNA based vaccines. They have figured out what part of the virus’s “code” is responsible for the “spikes” on the outside of the virus, and constructed a piece of “Messenger RNA” that can be injected into our bodies, asking our cells to become factories for this “spike” protein. Our immune systems then develop antibodies or “virus fighters” against the spike protein. When our bodies then encounter the virus, our immune system essentially coats the virus with antibodies and helps to destroy it, or eliminate its ability to infect us.
Simply put, the new Messenger RNA vaccines send a “Wanted” poster to our immune systems, which prepare antibodies and are ready to respond if they ever see this character in the future. It doesn’t keep us from getting infected, but it keeps us from getting too sick if we encounter the virus.
The Good News
The great news is that the scientific community was working for years on this type of vaccine as a potential treatment for other common diseases. They were able to put all that research to use to rapidly figure out the genetic code of the virus, isolate the “code” for the various proteins on the surface of COVID-19, and develop a way to get our bodies to take a small piece of that code to manufacture a piece of the virus and develop an immune response without getting the negative effects of the disease. It’s pretty cool when you think about it!
The two vaccines that are currently becoming available- Moderna and Pfizer- require cold storage to remain active, and it’s hard to make sure you keep things cold when you ship it to destinations all over the country. On top of it, Corning has developed a special vaccine flask, that helps keep vaccines safer, and helps speed the manufacturing process for this type of vaccine.
(Some vaccines need to be made in chicken eggs- we’re really lucky that this new vaccine doesn’t need to be made that way, or we would be out of eggs throughout the Country for an extended period of time!)
The coordination of so many pieces of the discovery, testing, mass manufacturing and distribution of the vaccines has been an incredible feat in itself. Now there is an equally big challenge to coordinate the distribution of the vaccines and making sure those that need them most get them as quickly as possible. Think of all the people needed to do the actual injections, and then add in everyone we need to keep the records straight of who has gotten what vaccine, how to follow up and ensure they get a second dose, and you can start to imagine how complicated the process is- there are a lot of moving parts besides the simple shot in your arm to consider.
Do we still need to wear masks?
Simply put, yes. Even if you get vaccinated, you still may be able to be a carrier for the virus- we just don’t know yet. Until we have more information and data, we will all need to wear masks- likely until at least the summer, if not longer.
Will this impact visitation?
We know how much you want to have visitation with your loved ones here at Chandler Hall, or want to come on campus to learn more about everything we have to offer. There are so many issues that still have to be worked out, as well as getting the vulnerable vaccinated. As soon as we know more, we will share it here on our website and by email if you are part of our email list. (You can join by clicking on the link below). We’re excited to see you- and we can’t wait to be able to see you with your loved ones here on campus! As soon as it’s safe, we will let you know!